
Genesiss Hospital |
Blogs

Premenstrual Syndrome (PMS)
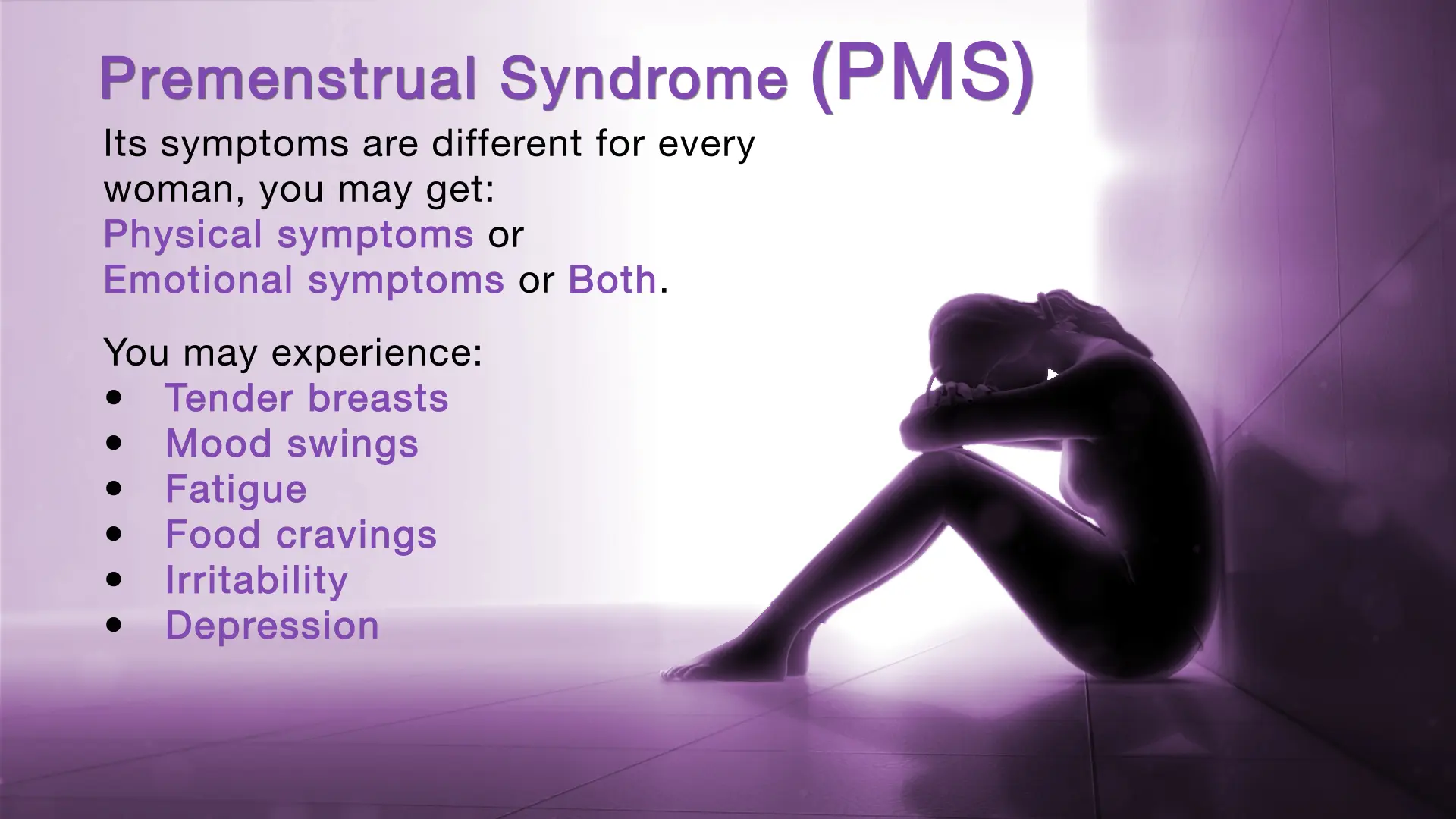
Understanding Premenstrual Syndrome (PMS) and How to Manage It
In the days leading up to their period, many women notice unexplained changes—mood swings, sudden cravings, bloating, or a general sense of unease. These symptoms can feel frustrating, especially when they interfere with daily life. Often, they are linked to premenstrual syndrome (PMS), a condition that affects both body and mind during the second half of the menstrual cycle. This guide explores the key signs of PMS and offers practical ways to manage it at home.
What is Premenstrual Syndrome (PMS)?
PMS refers to a set of physical, emotional, and behavioural symptoms that appear in the days before a period, usually after ovulation. Symptoms typically ease once menstruation begins. PMS is largely influenced by hormonal fluctuations, particularly changes in estrogen and progesterone.
The severity of PMS varies widely. Some people experience mild discomfort, while others have symptoms that disrupt daily life. With proper awareness and strategies, PMS can often be effectively managed.
Causes of PMS
While the exact cause is not fully understood, PMS is mainly related to hormonal changes during the menstrual cycle:
- After ovulation, estrogen and progesterone levels rise and then drop sharply if pregnancy does not occur.
- These shifts affect brain chemicals like serotonin, which influence mood, sleep, and appetite.
Other factors can intensify PMS, including:
- High stress levels
- Poor sleep
- Lack of physical activity
- Diet low in essential nutrients
- Increased sensitivity to hormonal changes
Symptoms of PMS
1. Emotional and Behavioural Symptoms:
- Irritability and mood swings
- Low mood or sadness
- Anxiety or restlessness
- Crying spells
- Loss of interest in regular activities
- Difficulty concentrating
- Sleep disturbances
- Changes in appetite
2. Physical Symptoms:
- Bloating and abdominal discomfort
- Breast tenderness or swelling
- Cramps
- Headaches or migraines
- Fatigue
- Joint or muscle aches
- Temporary weight gain due to water retention
- Skin changes, such as breakouts
- Digestive issues, including constipation or diarrhea
Managing PMS Symptoms at Home
1. Stay Physically Active:
- Walking, yoga, cycling, or swimming
- Improves mood, circulation, and reduces fatigue
2. Eat a Balanced Diet:
- Include whole grains, fruits, vegetables, legumes, and lean proteins
- Reduce salt, processed foods, sugar, and caffeine
- Drink plenty of water
3. Prioritise Sleep:
- Maintain a consistent sleep schedule
- Keep the bedroom cool, quiet, and dark
- Limit screen time before bed
4. Manage Stress:
- Practice deep breathing or meditation
- Spend time outdoors
- Engage in hobbies or relaxation activities
5. Use Heat Therapy:
- Warm compresses or heating pads for cramps
- Warm baths to ease muscle aches
6. Track Symptoms:
- Note the type, timing, and intensity of symptoms
- Helps identify patterns and effective management strategies
Medical Treatments for PMS
When home remedies are insufficient, medical treatment may be recommended:
- Hormonal therapy: Birth control pills, patches, or IUDs can stabilize hormone levels.
- Antidepressants: Prescribed for severe mood changes, irritability, or anxiety.
- Pain relief: NSAIDs or paracetamol for cramps and headaches.
- Diuretics: For managing bloating and fluid retention.
- Cognitive Behavioural Therapy (CBT): Helps manage emotional symptoms effectively.
When to Seek Medical Help
Consult a gynaecologist if:
- PMS symptoms interfere with work, relationships, or daily life
- Emotional changes are intense or persistent
- Physical discomfort is severe or unusual
- Symptoms change suddenly from one cycle to another
Tracking symptoms over several cycles can help provide clarity for a doctor. Early support helps manage PMS effectively and rules out other underlying conditions.
Frequently Asked Questions (FAQs)
Can PMS symptoms change with age?
Yes, PMS symptoms can change as a person gets older. They may become more noticeable or intense in the 30s and 40s, particularly as hormonal patterns shift in the years leading up to menopause. Common changes include stronger mood swings, increased bloating, or heightened breast tenderness.
Does hormonal birth control affect PMS?
Hormonal birth control can help reduce PMS symptoms by stabilising hormone levels and sometimes preventing ovulation. However, responses vary among individuals, and some may experience changes in symptom patterns or side effects.
Can PMS occur after menopause?
No, PMS only occurs in individuals who are still ovulating. After menopause, when periods stop, PMS symptoms should not appear. However, hormonal changes during menopause may cause symptoms that feel similar to PMS, such as mood changes or sleep disturbances.
What is the difference between PMS and PMDD?
PMDD (premenstrual dysphoric disorder) is a severe form of PMS. It causes intense mood swings, extreme irritability, sadness, or tension, and significantly interferes with daily life. PMDD usually requires medical evaluation and treatment.
Can PMS affect appetite or digestion?
Yes, PMS can impact appetite and digestion. Many individuals experience cravings for specific foods, bloating, constipation, or diarrhea due to hormonal changes that influence metabolism and digestive function.
Does PMS impact fertility?
No, PMS itself does not affect fertility. It occurs during regular menstrual cycles and is not a sign of fertility problems. However, conditions that may coexist with PMS, such as PCOS or endometriosis, can impact fertility and may require medical attention.
If PMS symptoms interfere with daily life, a consultation with a gynaecologist can help manage them effectively. Genesiss Multi-Speciality Hospital’s gynaecologists provide personalised guidance and treatment options to improve comfort, emotional well-being, and overall health.
Need medical care?
Book your appointment with our expert doctors in just a few clicks.
